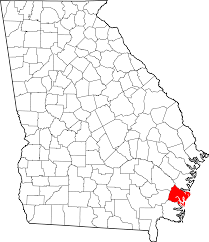
On December 17, 2019, the United States Attorney for the Southern District of Georgia announced that Brunswick, Georgia-based Medicaid provider Miracle Home Care, Inc. has been ordered to pay $9.7 million and the owner of Miracle Home Care, Inc., Shashicka Tyre-Hill of Brunswick has been ordered to pay $400,000 as a result of a civil complaint filed under the False Claims Act and the Georgia False Medicaid Claims Act. The Complaint, filed in July 2018, alleged that Miracle Home Care violated the False Claims Act and the Georgia False Medicaid Claims Act with claims for reimbursement for thousands of false or fraudulent non-emergency transportation and adult day health services. The government’s complaint alleged that Miracle also falsified thousands of records to cover up their false Medicaid claims. Miracle and Tyre-Hill consented to judgments against them and to the amounts of the judgments.
This Complaint was brought by the United States Attorney’s Office for the Southern District of Georgia and the Georgia Medicaid Fraud Control Unit. However, the federal False Claims Act and the Georgia False Medicaid Claims Act both have “qui tam” provisions that allow private individuals with knowledge of similar fraud against the United States or the State of Georgia to file a complaint on behalf of the United States and/or the State of Georgia. Under both the federal and Georgia False Claims Act qui tam provisions, the person bringing the case on behalf of the government, known as a relator, is entitled to between 15-25% of any recovery made by the Government, plus attorney fees and costs, if the Government intervenes in the case. If the Government declines to intervene, the relator has the right to continue to prosecute the case and is entitled to 25-30% of any recovery plus attorney fees and costs.
Commenting on the Miracle Home Care, Inc. judgments, Derrick L. Jackson, Special Agent in Charge for the U.S. Department of Health and Human Services Office of Inspector General said: “The act of falsifying records in order to steal millions of dollars from Medicaid, as alleged in this matter, will not be tolerated.” Similarly, United States Attorney for the Southern District of Georgia Bobby L. Christine stated: “This result sends a message to would-be unscrupulous providers of healthcare. Anyone who defrauds federally funded health care programs will be met with meaningful consequence. Our office is committed to continuing to partner with the Georgia Medicaid Fraud Control Unit to protect the integrity of the Georgia Medicaid Program.”
Frohsin Barger & Walthall congratulates and thanks the United States Attorney’s Office for the Southern District of Georgia, the Department of Health and Human Services, Office of Inspector General, the Georgia Office of the Attorney General and the Georgia Medicaid Fraud Control Unit for achieving this judgment. As members of the Southeast Georgia community, we applaud the hard work of these agencies to uncover and prosecute fraud perpetrated against our tax-payer funded health programs.
If you have questions about the False Claims Act or have knowledge about healthcare fraud, contact Frohsin Barger & Walthall.
Read the full Department of Justice Press Release here.





Talk with an Expert
Frohsin Barger & Walthall
Call 205.933.4006 or
Send us a Message