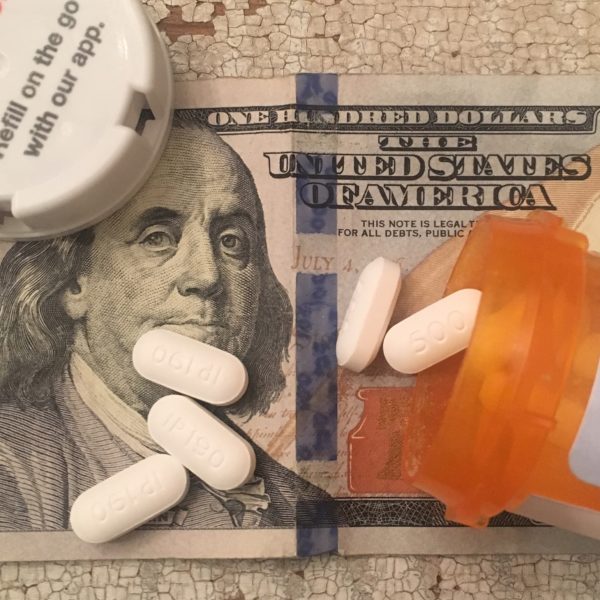
On Thursday, May 24, 2018, Pharmaceutical company Pfizer, Inc. (Pfizer), agreed to pay $23.85 million to resolve claims that it violated the False Claims Act by using a foundation as a conduit to pay kickbacks to Medicare patients who were prescribed Pfizer drugs. The kickbacks came in the form of Pfizer’s foundation paying the co-pay of Medicare beneficiaries taking three Pfizer drugs.
When a Medicare beneficiary obtains a prescription drug covered by Medicare Part B or Part D, the beneficiary may be required to make a partial payment, which may take the form of a copayment, coinsurance, or deductible (collectively copays). Congress included copay requirements in the Medicare program, in part, to encourage market forces to serve as a check on health care costs, including the prices that pharmaceutical manufacturers can demand for their drugs. Under the Anti-Kickback Statute and the False Claims Act, pharmaceutical companies cannot pay beneficiaries’ co-pay obligations to induce Medicare beneficiaries to purchase the company’s drugs.
The exact reasons for policies prohibiting drug companies from paying beneficiaries’ co-pays are demonstrated by Pfizer’s conduct. With respect to one of the Pfizer drugs involved in the settlement – Tikosyn, which treats arrhythmia in patients with atrial fibrillation or atrial flutter – Pfizer raised the wholesale acquisition cost of the drug by over 40 percent in the last three months of 2015. This drastic price increase would also increase the Medicare beneficiaries’ co-pay for Tikosyn and potentially prevent some patients from being able to afford the drug. Therefore, in order to raise the price of Tikosyn, but not lose Medicare beneficiaries’ business, Pfizer allegedly worked with the foundation to create and finance a fund for Medicare patients suffering from the condition treated by Tikosyn and coordinated the opening of the fund with the implementation of its price increase for the drug, and referred patients to the fund.
By doing so, Pfizer could raise the price of Tikosyn by over 40% (and consequently the portion of the drug price that the tax-payer funded Medicare program covers) and pay for the beneficiaries’ co-pay (typically 20%) and still make money because of the drastic initial price increase. As stated by United States Attorney for the District of Massachusetts Andrew E. Lelling: “Pfizer used a third party to saddle Medicare with extra costs. According to the allegations in today’s settlement agreement, Pfizer knew that the third-party foundation was using Pfizer’s money to cover the co-pays of patients taking Pfizer drugs, thus generating more revenue for Pfizer and masking the effect of Pfizer’s price increases. The Anti-Kickback Statute exists to protect Medicare, and the taxpayers who fund it, from schemes like these.”
In regard to the two other Pfizer drugs involved in the settlement, Sutent and Inlyta, which both treat renal cell carcinoma, the government alleged that, in order to generate revenue, and instead of giving Sutent and Inlyta to Medicare patients who met the financial qualifications of Pfizer’s existing free drug program, Pfizer used a third-party specialty pharmacy to transition certain patients to the foundation, which covered the patients’ Medicare copays. Pfizer allegedly made donations to the foundation to enable it to cover the copays of these patients and received confirmation from the foundation, via the specialty pharmacy, that the foundation funded the copays. Effectively, Pfizer charged United States taxpayers for drugs that they should have given away for free.
Harold H. Shaw, Special Agent in Charge, FBI Boston Division., commented: “[this] settlement demonstrates the FBI’s commitment to making sure patients receive, and the government pays for, health care that is not compromised by kickbacks. What Pfizer is accused of doing in this case—masking charitable contributions to increase company profits—violates the basic trust patients extend to the healthcare system and threatens the financial integrity of the Medicare program.”
To learn more about pharmaceutical kickbacks and how private whistleblowers can receive between 15-30 percent of a False Claims Act recovery, click here.
To speak with an attorney about pharmaceutical kickbacks, Medicare fraud or the False Claims Act, click here.





Talk with an Expert
Frohsin Barger & Walthall
Call 205.933.4006 or
Send us a Message