According to a Department of Justice press release, Freedom Health Inc., a Tampa, Florida-based provider of managed care services, and its related corporate entities (“Freedom Health”), agreed to pay $31,695,593 to resolve allegations that they violated the False Claims Act by engaging in illegal schemes to maximize their payment from the government in connection with their Medicare Advantage plans. In addition, the former Chief Operating Officer (COO) of Freedom Health Siddhartha Pagidipati, has agreed to pay $750,000 to resolve his alleged role in one of these schemes.
The allegations resolved by these settlements were originally brought by Darren D. Sewell, who was a former employee of Freedom Health in a lawsuit under the qui tam, or whistleblower, provisions of the Federal False Claims Act and the Florida False Claims Act. These statutes permit private parties with knowledge of fraud against the government to sue on behalf of the government for false claims and to receive a share of any recovery. Under the Federal False Claims Act, whistleblowers – known as relators – are entitled to 15 to 30 percent of the government’s recovery. Mr. Sewell’s share in this case has not yet been determined.
In the government’s lawsuit, it alleged that Freedom Health submitted or caused others to submit unsupported diagnosis codes to Medicare, which resulted in inflated reimbursements from 2008 to 2013 in connection with two of their Medicare Advantage plans operating in Florida. It also alleged that Freedom Health made material misrepresentations to CMS regarding the scope and content of its network of providers (physicians, specialists and hospitals) in its application to CMS in 2008 to expand in 2009 into new counties in Florida and in other states. The government’s settlement with Mr. Pagidipati resolves his alleged role in this latter scheme.
“Medicare Advantage insurers must play by the rules and provide Medicare with accurate information about their provider networks and their patients’ health,” said Chief Counsel to the Inspector General Gregory Demske of the Department of Health and Human Services Office of Inspector General (HHS-OIG). “OIG will investigate and hold managed care organizations accountable for fraud. Moving forward, the innovative CIA reduces the risks to patients and taxpayers by focusing on compliance issues unique to Medicare Advantage plans.”
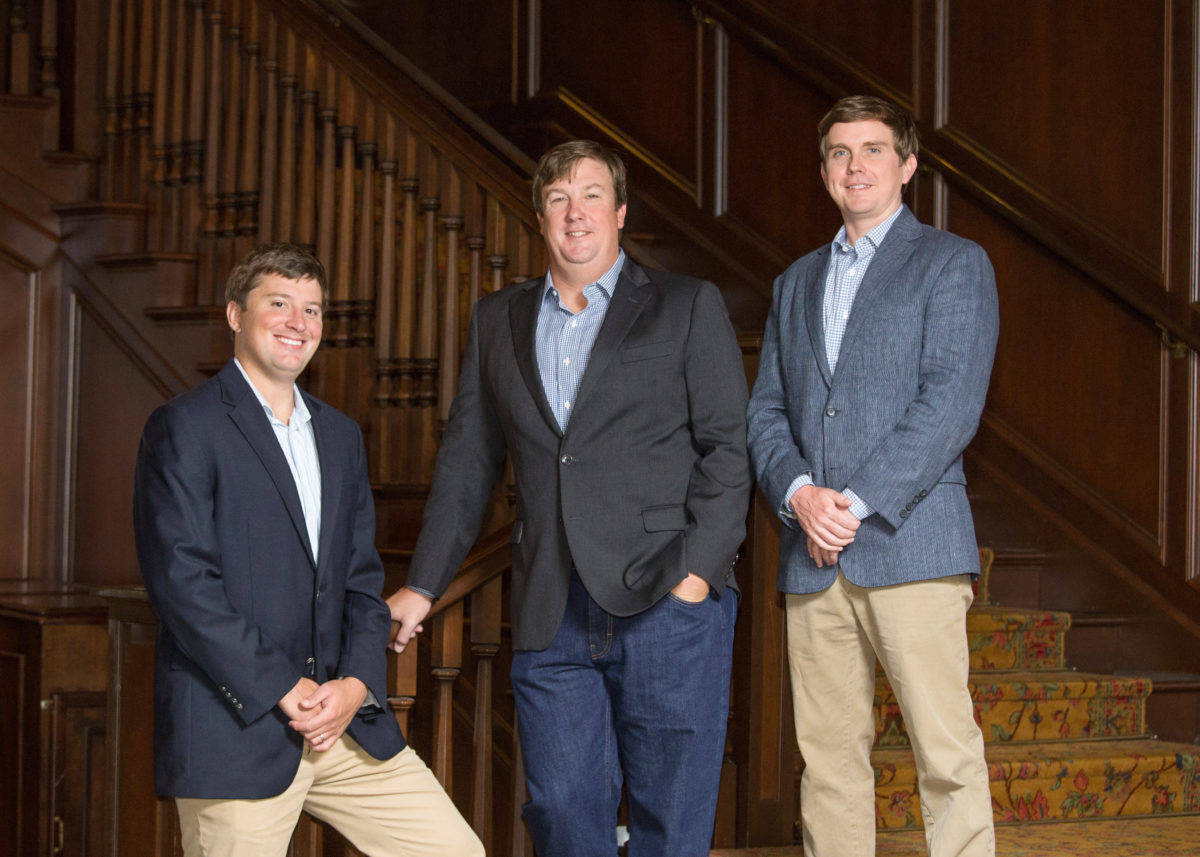
Frohsin Barger & Walthall would like to thank and congratulate the Department of Justice Civil Division’s Commercial Litigation Branch, The U.S. Attorneys’ Office for the Middle District of Florida, HHS-OIG, the Florida Office of the Attorney General as well as Mr. Sewell and his counsel for prosecuting this fraud and returning millions of dollars to the United States taxpayers.
To learn more about Medicare Fraud, click here






This scammer Siddhartha Pagidipati caused my mother untold suffering in 2008 when she found that none of the “Doctors” on the HMO were available. Freedom Health refused respond and drop her so she could enroll for straight Medicare. Her cancer treatment was delayed a month and she died.